Wicomico Middle instructor named Wicomico County’s Teacher of the Year
SALISBURY — Debbie Reynolds, a 7th grade World History teacher at Wicomico Middle School, was named the 2024-2025 Wicomico Teacher of the Year April 11 in an announcement at the Teacher of the …
SALISBURY — Airport improvements, educational funding and recent Maryland General Assembly wins were among topics discussed during the State of the County Address on April 11.
Wicomico …
SALISBURY — The Salisbury Fire Department has received a grant that will help it screen for one of the leading causes of death among firefighters in the United States.
Through the Maryland …
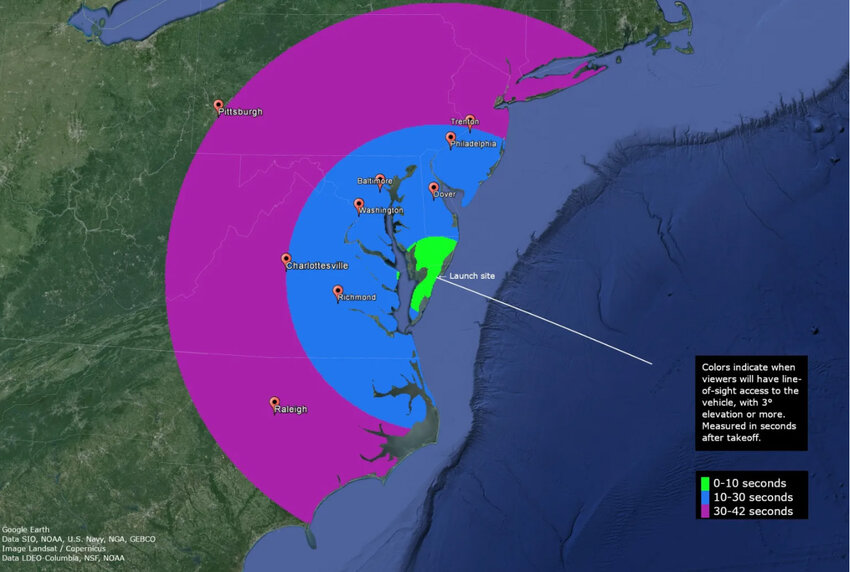
WALLOPS ISLAND, Va. — Three Black Brant IX sounding rockets for the Atmospheric Perturbations around Eclipse Path (APEP) mission are scheduled to launch from NASA’s Wallops Flight …
News

The Maryland State Highway Administration will conduct routine maintenance repairs on the Main Street (MD 991) Drawbridge over the Wicomico River in downtown Salisbury beginning Sunday, April 14, …

Public servant, scholar and Christian leader Dr. Gerald “Jerry” Regier will address the 12th annual...

DUNDALK, Md.— More than 1,000 small businesses have sought emergency federal loans to stay afloat following the March 26 collapse of the Francis Scott Key Bridge and closure of much of the Port …

TidalHealth announces a series of free skin cancer screenings for people without insurance...
The Take Down Tobacco initiative is a national campaign of activism that takes place each Spring...
E-Edition
View this issue of Salisbury Independent or browse other issues.
Salisbury
NASA and Salisbury University expand student opportunities with partnership
SALISBURY — Salisbury University and NASA have formally signed off on a partnership that will allow students to learn from some of the top experts in the space industry and expand the national …
Downtown Salisbury parking lot could become site of hotel and conference center
SALISBURY — The future of a downtown parking lot in Salisbury could become clearer with a proposed subrecipient agreement by its developer and the city.
Lot 10, situated next to a state …
Perdue Farms, Harry K Foundation, Food Bank of Delaware partner to deliver meals
As part of its Delivering Hope To Our Neighbors outreach, Perdue Farms joined the Harry K Foundation and the Food Bank of Delaware to help distribute meals to 764 food insecure children and families …
Neighbors
Registration open for virtual Alzheimer’s, Dementia Caregivers Conference
SALISBURY — MAC’s 2024 Virtual Alzheimer’s and Dementia Caregivers Conference, “Dementia: Navigating the Journey,” will be held Wednesday, April 24. CEU registration …
Former Ward Museum decoys to be on exhibit at Delmarva Discovery Museum
SALISBURY — For the first time since 2022, portions of the Salisbury University carving collection will be accessible to the public thanks to a partnership between SU’s Museum of Eastern …
VA Maryland reducing falls among veterans by focusing on hip muscles
Three million older adults find themselves being treated in emergency departments annually for injuries related to falling. In fact, falls are the leading cause of injury-related death and non-fatal …
Business
Telewire, Inc. invited to attend top technology event of the year
Telewire, Inc., a leading managed technology services provider, has received an exclusive invitation...
Groups begin investing $2 million in Delmarva chicken farming best management practices
Delmarva Chicken Association, the Alliance for the Chesapeake Bay, and the Nanticoke Watershed Alliance are partnering with chicken farmers to invest $2 million in cost-share programs to accelerate …
The Red Roost celebrates 50 years of food on the Eastern Shore
QUANTICO — A seasonal Eastern Shore restaurant in business for half a century recently opened back up to seafood lovers in search of the ultimate meal. The Red Roost opened during St. …
The 'American Pickers' looking for Maryland sites to use on its national TV show
The American Pickers are planning to return to Maryland to film episodes of The History Channel hit television series during the month of April.
"American Pickers" is a documentary series that …
Workshop to offer advice to heirs of property facing difficulties
PRINCESS ANNE — The University of Maryland Eastern Shore is offering an heirs’ property workshop Thursday, March 28 for Marylanders with family-owned property inherited through …
Business Insights

But an increasing, and unfortunate, issue that’s occurring is power lines being shot by hunters and gun enthusiasts...
Things to do

Outdoor Third Friday season starts this week with ‘Sustainable Spring’ theme
Spring is in the air, and Third Friday is back outdoors for the season starting this week.
Friday Night Live concert series features eight performances
The City of Salisbury’s Friday Night Live concert series is back for 2024 with a new twist.

St. Peter’s Third Friday Spring Bazaar Offers Oyster Fritter Supper & More
King Boys oysters, sides and refreshments are featured.
More Things to Do
Sports

NEWARK — Ryan O’Connor is Delaware’s most experienced quarterback.
But he knows he’s not the Blue Hens’ only current QB who’s proven he’s capable of …

Habitat for Humanity of Wicomico County will be hosting the Kitchens for Kitchens...

Dover Downs Results
Thursday, Feb. 15, 2024
1st - Clm 7500 Pace $6,000
7-Feherty (Ti Tetrick) 3.00 2.20 2.10
1-Trey's Charlie (Ge Napolitano Jr) 5.00 2.80
…

When, in July 2022, the world-renowned Ward Museum of Wildfowl Art abruptly had its doors closed and the immense art collection kept from public view, Delmarva — not just Salisbury, Wicomico …
I am a concerned Ocean Pines, Maryland, citizen who is appalled by the unsightly litter along our roads and waterways in our otherwise beautiful Eastern Shore. It’s time to actually do something to deal with this issue.
The following letter is in response to Michele Schlehofer’s opinion ("Wicomico Schools should not restrict access to books) which BaytoBayNews.com posted on Feb. 21.
This is a spot on, …
Concerns have been raised recently by Wicomico County Board of Education members about the process for initial selection and reconsideration of media resources, in particular books.
The current …
I am increasingly concerned that our County Board of Education is considering adopting policies which allow for broad personal bias to interfere with book collections development and book …
When the opening day of the 2024 Maryland General Assembly session was called to order, Delegate Sheree Sample-Hughes was the speaker pro tempore in the Maryland House of Delegates, the second-highest position for a member of the House Democratic Caucus.