Eastern Shore delegation members touch on education, housing and other topics during legislative forum
SALISBURY — A myriad of topics were discussed among Maryland’s Eastern Shore delegation members during the annual legislative wrap-forum hosted by the Salisbury Area Chamber of Commerce …
SALISBURY — A preliminary $198 million budget for Wicomico County includes $20.5 million for a new Fruitland Primary School but officials are divided on how it ultimately will be funded.
…
For the people living on Smith Island, the water matters.
But it’s about more than the beautiful views of the Chesapeake Bay from the picturesque island 10 miles from the mainland. The …
SALISBURY — Residents of a northern Wicomico County community continue to protest an upcoming Jeep-specific event planned for a nearby county-owned site off Connelly Mill Road in Delmar.
…
News
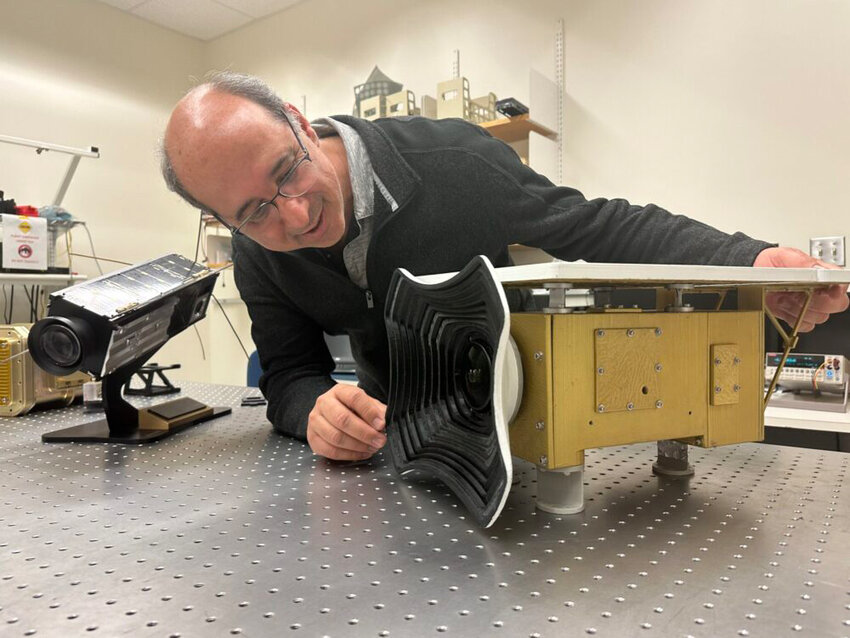
To better understand the ocean surface, NASA scientists went to the stars.
The Plankton, Aerosol, Cloud, ocean Ecosystem satellite launched into orbit Feb. 8 on a quest to better understand the microscopic content of Earth’s atmosphere and oceans.

TidalHealth Peninsula Regional honors the following four team members as 1st Quarter....

MAC’s 2024 Virtual Alzheimer’s and Dementia Caregivers Conference, “Dementia: Navigating...

SALISBURY — TidalHealth Primary Care and TidalHealth Specialty Care announce Tina Stade and Chrystal Willey are Team Members of the Month for March 2024.
Ms. Stade, Cancer Services …
A 64-year-old Wicomico County man has been indicted on 228 charges.
E-Edition
View this issue of Salisbury Independent or browse other issues.
Salisbury
Wicomico County Executive Julie Giordano gives State of the County address
SALISBURY — Airport improvements, educational funding and recent Maryland General Assembly wins were among topics discussed during the State of the County Address on April 11.
Wicomico …
NASA and Salisbury University expand student opportunities with partnership
SALISBURY — Salisbury University and NASA have formally signed off on a partnership that will allow students to learn from some of the top experts in the space industry and expand the national …
Downtown Salisbury parking lot could become site of hotel and conference center
SALISBURY — The future of a downtown parking lot in Salisbury could become clearer with a proposed subrecipient agreement by its developer and the city.
Lot 10, situated next to a state …
Neighbors
Diocese of Wilmington announces Eucharistic Congress: 'The Eucharist: Source and Summit' this fall
The Diocese of Wilmington has announced an upcoming major spiritual event — the Eucharistic Congress — scheduled for October 5, 2024, at the Roland E. Powell Convention Center in Ocean …
Community Players announce auditions for last show of season
Community Players of Salisbury’s last show of the 2023-2024 season will be the classic Cole Porter Musical “Kiss Me Kate” from June 21 to 23 at Wicomico High School Auditorium. …
Registration open for virtual Alzheimer’s, Dementia Caregivers Conference
SALISBURY — MAC’s 2024 Virtual Alzheimer’s and Dementia Caregivers Conference, “Dementia: Navigating the Journey,” will be held Wednesday, April 24. CEU registration …
Business
More than 1,000 small businesses seek aid amid Baltimore port closure
DUNDALK, Md.— More than 1,000 small businesses have sought emergency federal loans to stay afloat following the March 26 collapse of the Francis Scott Key Bridge and closure of much of the Port …
Telewire, Inc. invited to attend top technology event of the year
Telewire, Inc., a leading managed technology services provider, has received an exclusive invitation...
Groups begin investing $2 million in Delmarva chicken farming best management practices
Delmarva Chicken Association, the Alliance for the Chesapeake Bay, and the Nanticoke Watershed Alliance are partnering with chicken farmers to invest $2 million in cost-share programs to accelerate …
The Red Roost celebrates 50 years of food on the Eastern Shore
QUANTICO — A seasonal Eastern Shore restaurant in business for half a century recently opened back up to seafood lovers in search of the ultimate meal. The Red Roost opened during St. …
The 'American Pickers' looking for Maryland sites to use on its national TV show
The American Pickers are planning to return to Maryland to film episodes of The History Channel hit television series during the month of April.
"American Pickers" is a documentary series that …
Business Insights

But an increasing, and unfortunate, issue that’s occurring is power lines being shot by hunters and gun enthusiasts...
Things to do

Salisbury Zoo welcomes new deer
The Salisbury Zoo recently welcomed a second white-tailed deer, Rosie.

Kid-Friendly Silent Film Night at St. Peter’s
On May 3, at 7 p.m., St. Peter’s Episcopal Church will welcome world-renowned concert organist Peter Richard Conte in a kid-friendly …

Salisbury Zoo to host Earth Day celebration, Zoo Stampede 5K on Saturday
Families can learn about animals and the environment at the Salisbury Zoo’s annual Earth Day...
More Things to Do
Sports

NEWARK — Ryan O’Connor is Delaware’s most experienced quarterback.
But he knows he’s not the Blue Hens’ only current QB who’s proven he’s capable of …

Habitat for Humanity of Wicomico County will be hosting the Kitchens for Kitchens...

Dover Downs Results
Thursday, Feb. 15, 2024
1st - Clm 7500 Pace $6,000
7-Feherty (Ti Tetrick) 3.00 2.20 2.10
1-Trey's Charlie (Ge Napolitano Jr) 5.00 2.80
…

Dear Mayor Randy Tayor and Salisbury City Council members, on behalf of the 100-plus members of the Greater Salisbury Committee, I write you in regards to the recent discussions about development in …

The members of the Maryland-Delaware-DC Press Association are deeply concerned about the potential consequences of Maryland House Bill 1258 on local journalism.

When, in July 2022, the world-renowned Ward Museum of Wildfowl Art abruptly had its doors closed and the immense art collection kept from public view, Delmarva — not just Salisbury, Wicomico …
I am a concerned Ocean Pines, Maryland, citizen who is appalled by the unsightly litter along our roads and waterways in our otherwise beautiful Eastern Shore. It’s time to actually do something to deal with this issue.
The following letter is in response to Michele Schlehofer’s opinion ("Wicomico Schools should not restrict access to books) which BaytoBayNews.com posted on Feb. 21.
This is a spot on, …
Concerns have been raised recently by Wicomico County Board of Education members about the process for initial selection and reconsideration of media resources, in particular books.
The current …